ANA PROFILE
28/9/22
ICU BED NO. 2
S
B/l pedal edema SOB
Fever spikes
O
Pt c/c/c
Bp - 120/70
PR - 142
RR- 29
Temp-99.5
Spo2 - 94 at room air
A
Post streptococcal glomerulonephritis..??
IGA nephropathy..??
Infective endocarditis..??
P
1)INJ Augmentin 1.2gm iv BD
2)INJ lasix 40mg iv BD
3) NEB Duolin, Budocort 6th hourly
4) INJ neomol 1gm/iv/sos
5) TAB Azithromycin 500mg po bd
6) Betadine gargles tid
29/9/22
ICU BED NO. 2
S
B/l pedal edema SOB
Fever spikes
O
Pt c/c/c
Bp - 120/70
PR - 142
RR- 29
Temp-99.5
Spo2 - 94 at room air
A
Post streptococcal glomerulonephritis..??
IGA nephropathy..??
Infective endocarditis..??
P
1)INJ Augmentin 1.2gm iv BD
2)INJ lasix 40mg iv BD
3) NEB Duolin, Budocort 6th hourly
4) INJ neomol 1gm/iv/sos
5) TAB Azithromycin 500mg po bd
6) Betadine gargles tid
30/9/22
ICU BED NO. 2
S
Fever spikes +
Stools not passed
O
Pt c/c/c
Bp - 1110/70
PR - 128
RR- 29
Temp-100.6
Spo2 - 94 at room air
A
Post streptococcal glomerulonephritis..??
IGA nephropathy..??
Infective endocarditis..??
Polyserositis 2' to SLE
P
1)INJ Augmentin 1.2gm iv BD
2)INJ lasix 40mg iv BD
3) NEB Duolin, Budocort 6th hourly
4) INJ neomol 1gm/iv/sos
5) tab prednisolone 50mg po bd
6) Betadine gargles tid
7) inj pan 40 mg iv bd
1/10/22
ICU BED NO. 2
S
B/l pedal edema subsided
COUGH +
O
Pt c/c/c
Bp - 110/70
PR - 125
RR- 29
Temp-98.6
Spo2 - 94 at room air
A
Falreup of SLE
infective endocarditis
Drug induced
P
1)INJ CEFTRIAXONE 1GM IV BD
2)INJ PAN 40 MG IV OD
3) INJ LASIX 40 MG IV BD
4) INJ DERIPHYLLIN 100MG IV BD
5) INJ NEOMOL 1GM IV SOS
6) TAB PREDNISOLONE 50 MG PO BD
7) NEB BUDECORT 12TH HOURLY
2/10/22
ICU BED NO. 2
S
Action tremors +
FEVER SPIKES +
O
Pt c/c/c
Bp - 120/70
PR - 101
RR- 22
Temp-99.5
Spo2 - 94 at room air
A
FLARE UP SLE WITH
LUPUS NEPHRITIS
CNS LUPUS VASCULITIS
P
1) Iv fluids NS @30ml/hr
2) inj methyl Prednisone 750mg in 100ml NS IV OD
3) INJ. CEFTRIAXONE 1GM IV/BD
4) INJ. PAN 40 MG IV/OD
5) INJ. LASIX 40 MG IV OD
6) INJ.NEOMOL 1GM IV/SOS
7) INJ. DERIPHYLLIN 100MG IV/BD
8) INJ. TRAMADOL 100MG IN 100 ML NS IV/BD
9) TAB HCQ 200 MG PO/OD
10) TAB. PREDNISOLONE 30MG/PO/BD
11) TAB. DOLO 650 MG PO/TID
12) NEB . BUDECORT P/N 12TH HRLY
13) BP, PR, TEMP, 4TH HRLY CHARTING
3/10/22
ICU BED NO. 2
S
B/l pedal edema subsided
COUGH +
Pt c/c/c
Bp - 110/70
PR - 125
RR- 29
Temp-98.6
Spo2 - 94 at room air
A
Falreup of SLE
LUPUS NEPHRITIS
CNS vasculitis
P
1)INJ CEFTRIAXONE 1GM IV BD
2)INJ PAN 40 MG IV OD
3) INJ LASIX 40 MG IV BD
4) INJ DERIPHYLLIN 100MG IV BD
5) INJ NEOMOL 1GM IV SOS
6) TAB PREDNISOLONE 50 MG PO BD
7) NEB BUDECORT 12TH HOURLYSolved
8) IV fluids NS @50 ml/hr
9) inj methyl Prednisone IV OD
10) tab hcq200mg po od
11) oint t bact l/a bd
12) neosporin powder for l/a
4/10/22
ICU BED NO. 2
S
B/l pedal edema subsided
COUGH +
Pt c/c/c
Bp - 110/70
PR - 125
RR- 29
Temp-98.6
Spo2 - 94 at room air
A
Falreup of SLE
LUPUS NEPHRITIS
CNS vasculitis
P
1)INJ CEFTRIAXONE 1GM IV BD
2)INJ PAN 40 MG IV OD
3) INJ LASIX 40 MG IV BD
4) INJ DERIPHYLLIN 100MG IV BD
5) INJ NEOMOL 1GM IV SOS
6) TAB PREDNISOLONE 50 MG PO BD
7) NEB BUDECORT 12TH HOURLYSolved
8) IV fluids NS @50 ml/hr
9) inj methyl Prednisone IV OD
10) tab hcq200mg po od
11) oint t bact l/a bd
12) neosporin powder for l/a
08/10/22
S
No fever spikes
Pt c/c/c
Bp - 120/90
PR - 74
RR- 16
Temp-98
Spo2 - 98 at room air
A
Falreup of SLE
LUPUS NEPHRITIS
CNS vasculitis
P
1)TAB. PAN 40 MG PO OD
2)TAB. MCQ 200MG/PO/OD
3) TAB PREDNISOLONE 20 MG PO BD
4) TAB. AZORAN 50 MG PO BD
5) TAB. WARFARIN 5MG PO OD
6) TAB. WARFARIN 5MG PO OD
6) SYP. DULPHALAC 15 ML / PO/ TID
7) OINT - T - BACT L/A BD
8) CEBHYDRA LOTION L/A BD
9) NEOSPORIN POWDER L/A
First admission discharge summary
Age/Gender : 21 Years/Female
Address :
Discharge Type: Relieved
Admission Date: 27/09/2022 04:57 PM
Diagnosis
SYSTEMIC LUPUS ERYTHEMATOSUS WITH GLOMERULONEPHRITIC FLARE UP OF LUPUS NEPHRITIS ?CATASTROPHIC APLA SECONDARY TO SLE [LIBMAN SACKS ENDOCARDITIS
,CNS THROMBO EMBOLISM, AND RENAL FAILURE]
Case History and Clinical Findings
20 YR OLD FEMALE CAME ITH C/O B/L PEDAL EDEMA SINCE 15 DAYS HYPERPIGMENTED MACULES SINCE 15 DAYS
FEVER SINCE 15 DAYS
ABDOMINAL DISTENSION SINCE 8 DAYS DRY COUGH SINCE 7 DAYS
SORE THROAT SINCE 7 DAYS DECREASED APPETITE SINCE 7 DAYS SOB SINCE 5 DAYS
DECREASED URINE OUTPUT SINCE 3 DAYS CONSTIPATION SINCE 3 DAYS
HOPI -20 YEAR OLD FEMALE CAME WITH C/O OF B/L PEDAL EDEMA EXTENDING TILL THE KNEES PITTING TYPE SINCE 15DAYS
FOR WHICH SHE GOT MEDICAL HEALTH CHECKUP AND PRESCRIBED SOME MEDICATION [UNKNOWN] THEN HER PEDAL EDEMA GOT RESOLVED ALNG WITH FEVER SHE DEVELOPED HYPER PIGMENTED MACULES ON FACE LATER THEY STOPPED MEDICATIONS AFTER 2 DAYS SHE AGAIN HAD A COMPLAINT OF B/L PEDAL EDEMA AND FEVER ABDOMINAL DISTENSION ASSOCIATED WITH DRY COUGH AND DECREASED APPETITE SHE ALSO HAS COMPLAINTS OF DECREASED URINE OUTPUT AND CONSTIPATION SINCE 3 DAYS
PASSING STOOLS ONCE IN 3-4 DAYS N/K/C/O HTN DM THYROID CAD EPILEPSY TB
PERSONAL HISTORY DIET MIXED APPETITE LOST
BOWEL AND BLADDER MOVEMENTS DECREASED
FAMILY HISTORY NOT SIGNIFICNT
O/E-
PT WAS C/C/C
ON ADMISSION VITALS BP 110/70 MMHG
PR-79 BPM RR-19 CPM TEMP -98.8 F
CVS- APEX BEAT DISPLACED LATERALLY PALPABLE THRILL IN MITRAL AREA
LOUD S2 HEARD IN ALL AREAS NO S3 HEARD
PAN SYSTOLIC MURMUR AT MITRAL AREA
RS-
BAE DECREASED
RT INFRA SCAPULAR CREPTS PRESENT P/A-
SOFT NON TENDER WITH EMBILICUS NORMAL SHAPE AND INVERTED XIPHI UMBILICAL LENGTH 15 CM
UMBILICO PUBIC LENGTH 12 CM
ON PALPATION NO ORGANOMEGALY
CNS -B/L UPPER LIMB AND LOWER LIMB
HYPER TONIA WITH EXAGERATED DTR ,ABSENT ANKLE REFLEX PATELLAR CLONUS-
RT SIDE 4+
LT SIDE 3+
MOTOR POWER- 4/5 4/5
4/5 4/5
1/10/22
MMSE - DONE ON 1/10/22 ORIENTATION -
ORIENTED TO DAY,MONTH ,SEASON ,DATE -2 FLOOR ,HOSPITAL,DISTRICT,STATE ,COUNTRY-4 RECALL-2/3
ATTENTION AND CALCULATION-3/4 LANGUAGE -2 OBJECTS-2 SENTENCE-1
3 STAGE COMMAND -3 READING CLOSE YOUR EYES WRITING A SENTENCE -0
MODERATE COGNITIVE IMPAIRMENT COURSE IN HOSPITAL
28/09/22-
NEPHRO REFERAL I/V/O ELEVATED RENAL PARAMETERS AND ANASARCA
REFERAL NOTES-LVTS-,OBSTRUCTION -,HEMATURIA-,PYURIA-,YELLOWIS DISCOLORATION-
,NSAID ABUSE -,NATIVE MEDICATION - ADVICED TO CONTINUE THE SAME TREATMENT 28/09/22-
PULMO REFERAL I/V/O WHEEZE ,XRAY CHANGES [BL PLEURAL EFFUSION] ADVICED -INJ AUGMENTIN 1.2 GM IV/TID
INJ.LASIX 40 MG IV/BD NED DUOLIN
BUDECORT 6TH HOURLY IMJ NEOMOL 1GM IV/SOS BETADINE GARGLING TAB AZITHROMYCIN
GENERAL SURGERY REFERAL I/V/O BED SORE [1/10/22]
LE- TWO SMALL ULCERS NOTED EITHER SIDE OF INTERGLUTEAL CLEFT MEASURING 1X1 CM EACH
NO ACTIVE DISCHARGE
FLOOR -GRANULATION TISSUE,NO SLOUGH
EDGE SLOPING EDGES NO SURROUNDING INDURATION MARGINS -BLACKISH
ADVICED -TO MAINTAIN HYGEINE AND KEEP THE AREA DRY OINT T BACT FOR LA
NEOSPORIN POWDER FOR LA FREQUENT POSITION CHANGE AIR BED
29/09/22-
ENT REFERRAL WAS TAKEN I/V/O DYSPHONIA REFRAL NOTES-
O/E OF ORAL CAVITY- MUCOSA PALE TONGUE IS COATED
OROPHARYNX-BL GRADE 2 TONSILLAR HYPERTROPHY ,NO CONGESTION NECK-TRACHEA CENTRAL
LARYNGEAL FRAMEWORK NORMAL LARYNGEAL CREPITUS+
NOSE-
EXTERNAL FRAMEWORK NORMAL CAUDAL DISLOCATION-LEFT ANTERIOS MILD DNS -RIGHT
B/L NASAL MUCOSA -PALE TURBINATES AND FLOOR -NORMAL ROOMY NASAL CAVITIES
OE EAR-
B/L TYMPANIC MEMBRANE INTACT .,COL+ DIAGNOSIS-DYSPHAGIA UNDER EVALUATION NO ACTIVE ENT INTERVENTION
30/09/22-
REVIEW NEPHRO REFERAL-
USG KUB SHOWING BULKY LT KIDNEY WITH ALTERED ECHOTEXTURE ADVICED TAB AUGMENTIN
TAB PAN 40 MG OD TAB DOLO 650 MG TID 4/10/22-
DVL REFERAL I/V/O HYPERPIGMENTED MACULES NOTED OVER CHEEKS AND FOREHEAD
,NOSE ,CHIN EAR LOBULE ,RETROAURICULAR REGION [CONCHA SPARED], BOTH FOREARMS,BACK,UPPER CHEST
ORAL CAVITY- N
MULTIPLE HYPERPIGMENTED MACULES NOTED OVER BOTH THE PALMS DIAGNOSIS -POST INFLAMMATORY HYPERPIGMENTATION
ADVICED -CEBHYDRA LOTION LA/BD
REVIEW ENT REFERAL I/V/O DYSPHONIA [13/10/22]
ADVICED TO CONTINUE MEDICATION AS ADVICED BY PHYSICIAN WAIT AND WATCH
FOLLOWED BY SPEECH THERAPY
01/10/2022-
20 F WITH ANASRCA BL PEDAL EDEMA ,PLEURAL EFFUSION ,AND PERICARDIAL EFFUSION - RESOLVING
+RASH HEALED +FEVER
SKIN- HEALED RASHES +PAINLESS EMBOLI LIKE LESIONS [JANEWAY LESIONS] PT APPEARS COMFORTABLE
FEVER SPIKES PERSIST -FEVER CHART ANALYSIS-SEPTIC PTTERN ACTION TREMOR+B/L
REDUCTION IN TACHYCARDIA[HR 148->112] LIDLAG
HEALING BEDSORE ON BACK [BUTTOCK AREA]
ON 02/10/22-
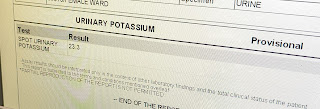
ANA PROFILE -ANTI dsDNA +++
ANTI HISTONE ,ANTINUCLEOSOME,ANTI KU AG++
MRI BRAIN- MULTIPLE HYPERINTENSITIES IN BRAIN PARENCHYMA F/S/O-VASCULITIS? USG ABDOMEN -MODERATE ASCITES
SLE DAI SCORE-30 POINTS S/O ACTIVE DISEASE
ON 3/10/22-
TACHYPNEA AND TACHYCARDIA SUBSIDED ACTION TREMOR DECREASED
0N 4/10/22
INJ UNFRACTIONATED HEPARIN 5000IU /IV/STAT
FOLLOWED BY INJ UNFRACTIONATED HEPARIN 5000 IU /SC/QID FOR 3 DAYS[GIVEN FOR 3 DAYS [TILL 6//10/22]]
TAB WARFARIN 5MG /PO/OD IS STARTED
TAB LASIX 40MG PO/BD STARTED ON 12/10/22
BLOOD TRANSFUSION WAS DONE ON 13/10/22
ONE PINT OF A+VE BLOOD WAS TRANSFUSED AFTER DOING THE BLOOD GROUPING AND TYPING AND CROSS MATCHING
TRANSFUSION STARTED AT 7;30 PM AND WAS COMPLETED BY 11;20 PM
HALF AND HOURLY MONITORING OF VITALS WAS DONE DURING THE PROCESS OF TRANSFUSION
PRE TRANSFUSION VITALS AND POST TRANSFUSION VITALS WERE MONITORED,PT WAS STABLE AND NO CHILLS,RIGORS,FEVER,MYALGIA DURING THE TRANSFUSION
Investigation
USG IMPRESSION[28/09/2022] MODERATE PERICARDIAL EFFUSION BILATERAL PLEURAL EFFUSION GROSS ASCITES
MRI BRAIN PLAIN WITH CSPINE SCREENING[ON 3/10/22] IMPRESSION-
DIFFUSE CEREBRAL AND CEREBELLAR ATROPHY
MULTIPLE SMALL ACUTE INFARCTS IN BOTH CEREBRAL HEMISPHERES-EMBOLIC SCREENING OF CERVICAL AND DORSAL SPINE APPEARS NORMAL
Treatment Given(Enter only Generic Name)
1] INJ AUGUMENTIN 1.2 GM IV/BD FOR 2 DAYS
2] INJ LASIX 40 MG IV/BD FOR 9 DAYS
3] NEB WITH DUOLIN BUDECORT
4] INJ NEOMOL 1GM IV/SOS
5] TAB AZITHROMYCIN 500 MG PO/OD FOR 2 DAYS
6] BETADINE GARGLES /TID
7] INJ DERIPHYLLINE 100 MG IV /BD FOR 7 DAYS
8] TAB PREDNISOLONE 50 MG PO/BD FOR 3 DAYS[STARTED ON 29/9/22 TO 1/10/22] TAB PREDNISOLONE 30 MG PO/BD FOR 1 DAY[STARTED ON 2/10/22 ]
TAB PREDNISOLONE 20 MG PO/BD FOR 11 DAYS[STARTED ON 3/10/22 ] 9]INJ PAN 40 MG IV/OD
10] INJ CEFTRIOXONE 1 GM IV/BD FOR 7 DAYS
11] INJ TRAMADOL 1 AMP IN 100 ML NA/IV/BD
12] INJ METHYL PREDNISOLONE 750 MG IN 100 ML NS/IV /OD FOR 3 DAYS[2/10/22 TO 4/10/22]
13] TAB HCQ 200 MG PO/OD[STARTED ON 2/10/22]
14] TAB DOLO 650 MG PO/TID
15] OINT T BACT FOR LA /BD
16] NEOSPORIN POWDER FOR LA
17] TAB AZORAN 50 MG PO/BD
18] SYP DULPHALAC 15 ML PO/TID
19] INJ UNFRATIONATED HEPARIN 5000 IU/SC/QID FOR 3 DAYS
20] TAB WARFARIN 5MG /PO/OD
21] CEBHYDRA LOTION LA /BD
Advice at Discharge
1] TAB HCQ 200 MG PER ORAL ONCE DAILY
2] TAB PREDNISOLONE 20 MG PER ORAL TWICE DAILY
3] TAB AZORAN 50 MG PER ORAL TWICE DAILY
4] TAB LASIX 40 MG PER ORAL TWICE DAILY
5] SYP SUCRALFATE 10 MLTHRICE DAILY
6] SYP DULPHLAC 15 ML PER ORAL THRICE DAILY
7] OINT TBACT LOCAL APPLICATION TWICE DAILY
8] CEBHYDRA LOTION LOCAL APPLICATION TWICE DAILY
9] NEOSPORIN LOCAL APPLICATION
Follow Up
REVIEW TO GM OPD ON TUESDAYS OR SOS
When to Obtain Urgent Care
IN CASE OF ANY EMERGENCY IMMEDIATELY CONTACT YOUR CONSULTANT DOCTOR OR ATTEND EMERGENCY DEPARTMENT.
Preventive Care
AVOID SELF MEDICATION WITHOUT DOCTORS ADVICE,DONOT MISS MEDICATIONS. In case
of Emergency or to speak to your treating FACULTY or For Appointments, Please Contact: For Treatment Enquiries Patient/Attendent Declaration : - The medicines prescribed and the advice regarding preventive aspects of care ,when and how to obtain urgent care have been explained to me in my own language
SIGNATURE OF PATIENT /ATTENDER SIGNATURE OF PG/INTERNEE SIGNATURE OF ADMINISTRATOR SIGNATURE OF FACULTY
Discharge Date Date:13/10/2022 Ward:AMC Unit:GM 2