Introduction:
During a one-year period, 47 [17.2%] of 274 spinal consultations seen by a single neurosurgeon were scheduled for “unnecessary surgery”.
Unquote:
https://pmc.ncbi.nlm.nih.gov/
In the early 1900s, Ernest Codman, an orthopedic surgeon from Boston, was the first clinician to systematically follow his patients long-term to track the “end-results” of their surgeries. He dedicated his life to recording the clinical misadventures and eventual outcomes of patients in his hospital, in order to improve quality of care.6
Unquote
Unquote:
a prospective observational study of 544 patients, 60% of the patients were recommended unnecessary spine surgery (USS) (6). This alarming statistic highlights the prevalence of USS and the need for a better understanding of its contributing factors and potential solutions. Several factors have been identified that contribute to the issue of USS. One of the primary etiologies is the overreliance on MRI findings. MRI is not a reliable tool for identifying the source of pain in patients with back or neck pain because degenerative findings are common in asymptomatic patients (7). This has been well established in the medical community since Jensen et al. published their findings in the New England Journal of Medicine in 1994 (8). They found that 52% of the patients without low back pain had disc bulge at least in one level, 27% had a disc protrusion, and 1% had a disc extrusion.
Unquote:
Our patient centred learning experiences in case reports:
Case 1:
Charcot's joints post spinal surgery:
Case 2:
Lumbar surgery done and cervical vertebral surgery under consideration: https://
Case 3:
Patient of stroke with paralysis underwent spinal surgery for cervical myelopathy as no cranial brain MRI was done but only a cervical spine MRI was done during the first stroke during 2017! Subsequently during another recurrence of the stroke they again did the lumbar spine MRI but this time also did a cerebral MRI and realised it was all along a stroke and left his lumbar vertebrae alone. Currently in October 2024 he has had another stroke.
Data shared in CBBLE PaJR during the third clinical encounter:
[29/10, 15:36] CBBLE: 60M with sudden stroke and left hemiparesis in 2017 went to a nursing home who did his spinal MRI and not his brain MRI and then operated him for his incidental cervical discs!
[29/10, 15:39] CBBLE: ICU 1, 60M In 2020 they wanted to operate his lumbar discs too but also this time did his brain MRI and may have then figured out the 2017 issue!
[29/10, 15:40] CBBLE: 60M ICU 1 with second stroke causing right hemiparesis this time along with drowsiness
[29/10, 15:40] CBBLE: 60M cranial MRI this time
[29/10, 15:48] CBBLE: 60M ICU 1 cranial MRI this time. Metabolic syn risk factors, trunkal obesity, smoking and alcohol
Warts and all EMR summary (written by someone who perhaps wasn't able to make any attempt to learn more due to his her personal situational context inspite a lot more having been shared in CBBLE as above):
Age/Gender : 60 Years/Male
Address :
Discharge Type: Relieved
Admission Date: 24/10/2024 03:45 PM
Diagnosis
CVA SECONDARY TO ACUTE INFRACT WITH FEW TINY HEMORRHAGIC FOCI INVOLVING LEFT INTERNAL CAPSULE (CAUDATE HEAD , PUTMEN , GLOBUS PALLIDUS ANTERIOR LIMB) SEIZURES SECONDARY TO CHRONIC INFRACT IN RIGHT FRONTAL , PARIETOTEMPORAL
LOBES , RIGHT EXTERNAL CAPSULE AND BASAL GANGLIA
RECURRENT CVA SECONDARY TO NON COMPLIANCE TO DRUGS / ALCOHOL AND TOBACCO HARMFUL USE
ASPIRATION PNEUMONIA (RESOLVING) K/C/O TYPE II DM AND HTN SINCE 6 Years
Address :
Discharge Type: Relieved
Admission Date: 24/10/2024 03:45 PM
Diagnosis
CVA SECONDARY TO ACUTE INFRACT WITH FEW TINY HEMORRHAGIC FOCI INVOLVING LEFT INTERNAL CAPSULE (CAUDATE HEAD , PUTMEN , GLOBUS PALLIDUS ANTERIOR LIMB) SEIZURES SECONDARY TO CHRONIC INFRACT IN RIGHT FRONTAL , PARIETOTEMPORAL
LOBES , RIGHT EXTERNAL CAPSULE AND BASAL GANGLIA
RECURRENT CVA SECONDARY TO NON COMPLIANCE TO DRUGS / ALCOHOL AND TOBACCO HARMFUL USE
ASPIRATION PNEUMONIA (RESOLVING) K/C/O TYPE II DM AND HTN SINCE 6 Years
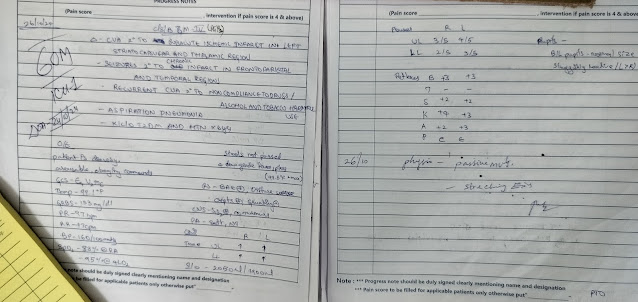
Case History and Clinical Findings
C/O SUDDEN ONSET OF RIGHT SIDED WEAKNESS ASSOCITED WITH SLURRING OF SPEECH SINCE 8 :00 AM ON 23 /10/2024
HOPI :
PATIENT WAS APPARENTLY ALRIGHT TILL 8 AM ON 23/10/24 , THEN HE DEVELOPED SUDDEN ONSET OF RIGHT SIDED WEAKNESS , NON PROGRESSIVE ASSOCIATED WITH UNCONTROLLED MOVEMENTS OF RIGHT UPPER AND LOWER LIMBS
C/O SLURRING OF SPEECH SINCE 8 AM ON 23/10/24 A/W DROOLING OF SALIVA H/O URINARY INCONTINENCE + SINCE YESTERDAY
H/O SOB GRADE 3-4 MMRC
NO H/O FEVER , VOMITING , NAUSEA , PAIN ABDOMEN , CHEST PAIN , PALPITATIONS , LOOSE STOOLS
PAST HISTORY :
K/C/O CVA 6 YEARS AGO AND WAS TREATED SURGICALLY (DOCUMENTS UNAVAILABLE ) K/C/O TYPE II DM AND HTN SINCE 6 YEARS
NO OTHER COMORMIDITIES PERSONAL HISTORY:
APPETITE LOST CONSTIPATION + INCONTINENCE +
CHRONIC ALCHOLIC SINCE 30 YEARS 90 ML/DAY TOBACCO SNUFFING 10-18 BEEDIS / DAY SINCE 6 YEARS FAMILY HISTORY :
H/O CVA FOR MOTHER GENERAL EXAMINATION:
MILD PALLOR +
NO ICTERUS CYANOSIS CLUBBING LYMPHADENOPATHY OEDEMA BP: 180/110 MMHG
RR:28 CPM PR: 88BPM
TEMPERATURE: 98.6F SPO2: 93% AT RA GRBS:133 MG/DL
CVS: NO THRILLS, S1S2 +, NO MURMURS
RS: BAE+, NVBS , BILATERAL DIFFUSE COARSE CREPTS PRESENT , DIFFUSE GRUNTING PRESENT
PER ABDOMEN: SOFT , NON TENDER CNS :
PATIENT IS DROWSY SPPECH - INCOHERENT GLASGOW SCALE:E4V2M6 REFLEXES:- RT LT
BICEPS :- 3+ 3+
TRICEPS :- - - KNEES :- 3+ +3
ANKLE :- +2 +3
SUPINATOR:- +2 +2
PLANTAR - EXTENSION ; EXTENSION
PUPILS- B/L NORMAL IN SIZE , REACTIVE TO LIGHT EQUALLY
TONE- RIGHT AND LEFT BOTH UPPERLIMBS AND LOWER LIMBS INCREASED POWER-RIGHT LEFT
UL 3/5 ; 4/5 LL 2/5 ; 3/5
COURSE IN THE HOSPITAL :A 60 YEAR MALE CAME WITH C/O SUDDEN ONSET OF RIGHT SIDED WEAKNESS ASSOCITED WITH SLURRING OF SPEECH SINCE 8 :00 AM ON 23 /10/2024. VITALS AT PRESENTATION BP- 180/110 MMHG, PR- 88 bpm, RR-28 CPM, SPO2- 93%. PATIENT WAS PROVISIONALLY DIAGNOSED AS CVA SECONDARY TO ACUTE ISCHEMIC STROKE IN LEFT CAPSULOGANGLIONIC REGION; SEIZURES SECONDARY TO OLD INFARCT IN TEMPORAL AND FRONTOTEMPORAL AND PARIETAL REGIONS; RECURRENT CVA SECONDARY TO NON-COMPLIANCE TO DRUGS / ALCHOLOL AND TOBACCO HARMFUL USE; ASPIRATION PNEUMONIA; K/C/O TYPE II DM AND HTN SINCE 6 YEARS, (BASED ON HISTORY, CLINICAL EXAMINATION, INVESTIGATIONS AND OUTSIDE CT SCAN REPORTS). PATIENT WAS STARTED ON ANTICONVULSANTS AND DUAL ANTIPLATELETS. ON ADMISSION GCS WAS E4V2M6 WHICH GRADUALLY IMPROVED TO E4V3M6. ANTIBIOTICS WAS STARTED ON 25/10/24 AND CONTINUED FOR 7DAYS. 2DECHO WAS WAS DONE ON 25/10/24, WHICH SHOWED (EF = 65%), SEVERE CONCENTRIC LVH +, NO RWMA , MODERATE TR + WITH PAH, (ECCENTRIC TR +), MILD AR +. REVIEW 2D ECHO DONE ON 28/10/24 SEVERE CONCENTRIC LVH +. NO RWMA ,PARADOXICAL IVS, MILD TR + NO PAH, TRIVIAL MR/AR +, EF = 59 % , GOD LV SYSTOLIC FUNCTION, GRADE I DIASTOLIOC DYSFUNCTION, NO PE / LV CLOT , IVC SIZE -
1.0 CMS , COLLAPSING, ? MILD APEX HYPOKINESIA. ON 29/10/24, PATIENTS GCS SUDDENLY DROPPED TO E3V2M5 AND HAD RESPIRATORY DISTRESS. OXYGEN SUPPORT WAS INITIATED. MRI BRAIN WAS DONE ON 29/10/24 WHICH SHOWED ACUTE INFARCT WITH FEW TINY INTERNAL HAEMORRHAGE FOCI SEEN INVOLVING THE LEFT CAUDATE HEAD,PUTAMEN,GLOBUS PALLIDUS, ANTERIOR LIMB OF INTERNAL CAPSULE.SUBTLE MASS EFFECT CAUSING MILD EFFACEMENT OF FRONTAL HORN OF LEFT LATERAL VENTRICLE AND MIDLINE SHIFT OF 2mm TO RIGHT; LARGE CHRONIC ISCHAEMIC INFARCT WITH RAREAS OF NEUROPARENCHYMAL LOSS OF GLIOSIS SEEN INVOLVING THE RIGHT PARIETO TEMPORAL LOBES; LARGE AREAS OF GLIOSIS ALSO SEEN IN RIGHT FRONTAL LOBE WHITE MATTER, RIGHT EXTERNAL CAPSULR AND BASAL GANGLIA; FEW CHRONIC LACUNAR INFARCTS IN B/L BASAL GANGLIA AND RIGHT THALAMUS, PO
NS; MILD TO MODERATE CHRONIC PERIVENTRICULAR AND DEEP WHITE MATTER MICROVASCULAR ISCHAEMIC CHANGES. HENCE IN VIEW OF HEMORRHAGIC TRANSFORMATION OF THE INFARCT, DUAL ANTIPLATELETS WERE REPLACED WITH SINGLE ANTIPLATELETS. PATIENTS' BLOOD PRESSURES REMAINED HIGH EVEN ON ARBs, BETA BLOCKERS, CCBs AND DIURETICS. HENCE ALPHA BLOCKERS WERE INITIATED AND BLOOD PRESSURES WERE GRADUALLY GOT UNDER CONTROL. DURING THE COURSE PATIENT WAS TREATED WITH ANTIHYPERTENSIVES, ANTICONVULSANTS, NEBULISATIONS, MULTIVITAMINS, PSYCHOSTIMULANTS, ANTIBIOTICS AND OTHER SUPPORTIVE TREATMENT.PATIENT IMPROVED CLINICALLY AND IS HENCE BEING DISCHARGED IN A HEMODYNAMICALLY STABLE CONDITION.
Investigation
HbA1c 6.2 %
HAEMOGLOBIN 16.8 gm/dl TOTAL COUNT 11,400 cells/cumm NEUTROPHILS 69 % LYMPHOCYTES 24 % EOSINOPHILS 01 % MONOCYTES 06 % BASOPHILS 00 %PCV 44.7 vol % M C V 82.0 flM C H 30.0 pg M C H C 37.6 % RDW-CV 13.2 % RDW-SD 40.2 flRBC COUNT 5.45
millions/cumm PLATELET COUNT 2.35 lakhs/cu.mm ceSMEARRBC Normocytic normochromic WBC leukocytosis PLATELETS AdeqauteHEMOPARASITES No hemoparasites seen IMPRESSION Normocytic normochromic bloodpicture with leukocytosis
Prothrombin Time 17 Sec INR 1.2 APTT TEST 33 Sec
RBS 114 mg/dl.
RFT 24-10-2024 05:54:PMUREA 42 mg/dl 42-12 mg/dlCREATININE 1.4 mg/dl 1.3-0.9 mg/dlURIC
ACID 6.3 mmol/L 7.2-3.5 mmol/LCALCIUM 10.2 mg/dl 10.2-8.6 mg/dlPHOSPHOROUS 4.0 mg/dl 4.5-
2.5 mg/dlSODIUM 140 mmol/L 145-136 mmol/LPOTASSIUM 3.4 mmol/L. 5.1-3.5 mmol/L.CHLORIDE 103 mmol/L 98-107 mmol/L
LIVER FUNCTION TEST (LFT) 24-10-2024 05:54:PMTotal Bilurubin 1.43 mg/dl 1-0 mg/dlDirect Bilurubin 0.40 mg/dl 0.2-0.0 mg/dlSGOT(AST) 21 IU/L 35-0 IU/LSGPT(ALT) 11 IU/L 45-0
IU/LALKALINE PHOSPHATASE 77 IU/L 119-56 IU/LTOTAL PROTEINS 6.4 gm/dl 8.3-6.4
gm/dlALBUMIN 3.9 gm/dl 4.6-3.2 gm/dlA/G RATIO 1.57
COMPLETE URINE EXAMINATION (CUE) 24-10-2024 05:54:PMCOLOUR Pale yellowAPPEARANCE ClearREACTION AcidicSP.GRAVITY 1.010ALBUMIN ++++SUGAR NilBILE SALTS NilBILE PIGMENTS NilPUS CELLS 3-6EPITHELIAL CELLS 2-4RED BLOOD CELLS NilCRYSTALS NilCASTS NilAMORPHOUS DEPOSITS AbsentOTHERS Nil
HBsAg-RAPID 24-10-2024 06:29:PM Negative
Anti HCV Antibodies - RAPID 24-10-2024 06:29:PM Non Reactive
RFT 25-10-2024 11:32:PMUREA 45 mg/dl 42-12 mg/dlCREATININE 1.2 mg/dl 1.3-0.9 mg/dlURIC
ACID 6.3 mmol/L 7.2-3.5 mmol/LCALCIUM 10.1 mg/dl 10.2-8.6 mg/dlPHOSPHOROUS 4.6 mg/dl 4.5-
2.5 mg/dlSODIUM 134 mmol/L 145-136 mmol/LPOTASSIUM 3.1 mmol/L. 5.1-3.5 mmol/L.CHLORIDE 101 mmol/L 98-107 mmol/L
HEMOGRAM
HAEMOGLOBIN 16.1 gm/dlTOTAL COUNT 12,400 cells/cumm NEUTROPHILS 78 %
LYMPHOCYTES 16 % EOSINOPHILS 02 % MONOCYTES 04 % BASOPHILS 00 %PCV 44.8 vol % M C V 85.9 fl M C H 30.9 pgM C H C 35.9 % RDW-CV 14.0 % RDW-SD 47.6 fl RBC COUNT 5.2
millions/cumm PLATELET COUNT 2.6 lakhs/cu.mm SMEARRBC Normocytic normochromic WBC increased on smear PLATELETS Adeqaute HEMOPARASITES No hemoparasites seen IMPRESSION Normocytic normochromic withleukocytosiS
LIPID PROFILE
Total Cholesterol 185 mg/dl Triglycerides 165 mg/dl HDL Cholesterol 45 mg/dl LDL Cholesterol 107 mg/dl.VLDL * 33.0 mg/dl
SERUM ELECTROLYTES
SODIUM 139 mmol/L POTASSIUM 3.5 mmol/L CHLORIDE 102 mmol/L CALCIUM IONIZED 1.17
mmol/L
ABG 25-10-2024 11:32:PMPH 7.43PCO2 33.8PO2 63.5HCO3 22.1St.HCO3 23.4BEB -1.0BEecf - 1.6TCO2 42.1O2 Sat 89.7O2 Count 19.9
SERUM ELECTROLYTES (Na, K, C l) 26-10-2024 06:29:PMSODIUM 139 mmol/L 145-136
mmol/LPOTASSIUM 3.5 mmol/L 5.1-3.5 mmol/LCHLORIDE 102 mmol/L 98-107 mmol/LRFT 26-10-
2024 11:39:PMUREA 43 mg/dl 42-12 mg/dlCREATININE 1.1 mg/dl 1.3-0.9 mg/dlURIC ACID 4.7
mmol/L 7.2-3.5 mmol/LCALCIUM 10.1 mg/dl 10.2-8.6 mg/dlPHOSPHOROUS 3.9 mg/dl 4.5-2.5
mg/dlSODIUM 135 mmol/L 145-136 mmol/LPOTASSIUM 3.6 mmol/L. 5.1-3.5 mmol/L.CHLORIDE 99
mmol/L 98-107 mmol/L HEMOGRAM
HAEMOGLOBIN 16.2 gm/dl TOTAL COUNT 10,900 cells/cummNEUTROPHILS 78 %
LYMPHOCYTES 13 %EOSINOPHILS 01 % MONOCYTES 08 %BASOPHILS 00 % PCV 45.5 vol % M C V 87.0 fl M C H 30.9 pgM C H C 35.5 % RDW-CV 14.0 % RDW-SD 47.7 fl RBC COUNT 5.2
millions/cumm PLATELET COUNT 2.5 lakhs/cu.mm SMEARRBC Normocytic normochromicWBC With in normal limits PLATELETS Adeqaute HEMOPARASITES No hemoparasites seen IMPRESSION Normocytic normochromic bloodpicture
RFT 27-10-2024 11:55:PMUREA 51 mg/dl 42-12 mg/dlCREATININE 0.9 mg/dl 1.3-0.9 mg/dlURIC
ACID 4.0 mmol/L 7.2-3.5 mmol/LCALCIUM 10.0 mg/dl 10.2-8.6 mg/dlPHOSPHOROUS 3.6 mg/dl 4.5-
2.5 mg/dlSODIUM 136 mmol/L 145-136 mmol/LPOTASSIUM 3.8 mmol/L. 5.1-3.5 mmol/L.CHLORIDE 101 mmol/L 98-107 mmol/L
HEMOGRAM
HAEMOGLOBIN 16.2 gm/dl TOTAL COUNT 10,400 cells/cumm NEUTROPHILS 70 % LYMPHOCYTES 20 % EOSINOPHILS 03 % MONOCYTES 07 % BASOPHILS 00 % PCV 46.3 vol % M C V 86.8 fl M C H 30.4 pg M C H C 35.0 % RDW-CV 14.1 % RDW-SD 48.0 fl RBC COUNT 5.34
millions/cumm PLATELET COUNT 2.85 lakhs/cu.mm SMEARRBC Normocytic normochromic WBC With in normal limits PLATELETS Adequate in number and distribution HEMOPARASITES No hemoparasites seen IMPRESSION Normocytic normochromic bloodpicture
ABG 28-10-2024 09:17:AMPH 7.42PCO2 31.8PO2 78.4HCO3 20.4St.HCO3 22.2BEB -2.6BEecf - 3.4TCO2 39.2O2 Sat 94.7O2 Count 20.2
HEMOGRAM 29/10/24
HB-17.2 gm/dl TOTAL COUNT 13,800 cells/cumm NEUTROPHILS 82 % LYMPHOCYTES 10 % EOSINOPHILS 00 % MONOCYTES 08 % BASOPHILS 00 % PCV 47.0 vol%M C V 86.0 fl M C H
31.4 pg M C H C 36.5 %RDW-CV 14.0 % RDW-SD 48.2 fl RBC COUNT 5.46 millions/cumm PLATELET COUNT 3.0 lakhs/cu.mmSMEARRBC Normocytic normochromic WBC increased in count PLATELETS Adequate in number and distribution HEMOPARASITES No hemoparasites seen IMPRESSION Normocytic normochromic bloodpicturewith neutrophilic leukocytosis .
HEMOGRAM 30 /10/24 HB-16.5 GM/DL
TLC-14,500 PCV-46.8 VOL%
PLATELET COUNT-2.80 MILLIONS/CUMM RBC COUNT -5.38 MILLIONS/CUMM
SERUM ELECTROLYTES 30/10/24 SODIUM-135 MMOL/L POTASSIUM-4.2 MMOL/L CHLORIDE- 101 MMOL/L
2D ECHO DONE 25/10/24 TACHYCARDIA DURING STUDY SEVERE CONCENTRIC LVH + 1.49 CMS
NO RWMA , MODERATE TR + WITH PAH , RV SP= 42 + 10 = 52 MMHG (ECCENTRIC TR +) MILD AR + (AR -PHT - 750 MSEC )
TRIVIAL MR + (ECCENTRIC MR +) SCLEROTIC AV , NO AS / MS , IAS INTACT EF = 65 % , GOD LV SYSTOLIC FUNCTION GRADE I DIASTOLIOC DYSFUNCTION
NO PE / LV CLOT
REVIEW 2D ECHO DONE ON 28/10/24 SEVERE CONCENTRIC LVH + 1.49 CMS NO RWMA ,PARADOXICAL IVS
MILD TR + NO PAH , RV SP = 37 + 5 = 42 MMHG TRIVIAL MR/AR +
SCLEROTIC AV , NO AS / MS , IAS INTACT
EF = 59 % , GOD LV SYSTOLIC FUNCTION GRADE I DIASTOLIOC DYSFUNCTION
NO PE / LV CLOT , IVC SIZE -1.0 CMS , COLLAPSING
? MILD APEX HYPOKINESIA
MRI BRAIN DONE ON 29/10/24
IMPRESSION: ACUTE INFARCT WITH FEW TINY INTERNAL HAEMORRHAGE FOCI SEEN INVOLVING THE LEFT CAUDATE HEAD,PUTAMEN,GLOBUS PALLIDUS, ANTERIOR LIMB OF INTERNAL CAPSULE.SUBTLE MASS EFFECT CAUSING MILD EFFACEMENT OF FRONTAL HORN OF LEFT LATERAL VENTRICLE AND MIDLINE SHIFT OF 2mm TO RIGHT
LARGE CHRONIC ISCHAEMIC INFARCT WITH RAREAS OF NEUROPARENCHYMAL LOSS OF GLIOSIS SEEN INVOLVING THE RIGHT PARIETO TEMPORAL LOBES. LARGE AREAS OF GLIOSIS ALSO SEEN IN RIGHT FRONTAL LOBE WHITE MATTER, RIHT EXTERNAL CAPSULR AND BASAL GANGLIA,
FEW CHRONIC LACUNAR INFARCTS IN B/L BASAL GANGLIA AND RIGHT THALAMUS, PONS MILD TO MODERATE CHRONIC PERIVENTRICULAR AND DEEP WHITE MATTER MICROVASCULAR ISCHAEMIC CHANGES.
HEMOGRAM ON 31/10/24 HB- 14.7 GM/DL
TLC- 10900
PCV- 41.7
RBC- 4.75
PLATELET- 2.49
RFT ON 31/10/24 UREA- 80
CREATININE- 0.9
URIC ACID- 4.2
CAL;CIUM- 9.1
PHOSPHOROUS- 3.40
SODIUM- 135
POTASSIUM - 4.5
CHLORIDE- 102
HEMOGRAM ON 1/11/24 HB- 14.8
TLC- 9700
PCV- 41.5
RBC- 4.78
PLATELET- 2.58
SERUM ELECTROLYTES ON 1/11/24 SODIUM- 135
POTASSIUM- 4.2
CHLORIDE- 104
IONIZED CALCIUM- 1.19
Treatment Given(Enter only Generic Name)
RT FEEDS - WATER 100 ML 2 ND HRLY AND MILK 200 ML 4 TH HRLY INJ. AUGMENTIN 1.2 G IV TID
INJ METROGYL 500 MG IV/ TID INJ. THIAMINE 200 MG IV / BD
INJ. OPTINEURON 1 AMPULE IN 100 ML NS IV / OD TAB. LEVEPIL 500 MG RT / BD
TAB. STROCIT PCVS RT/ BD TAB. CINOD 10 MG RT/BD TAB. TELMA 40 MG RT/BD TAB. MET XL 25 MG RT / OD
SYP. POTCHLOR 15 ML RT /TID SYP.LACTULOSE 15 ML RT/TID
NEB WITH IPRAVENT AND BUDECORT -M 12 TH HRLY AIR BED AND HEAD ELEVATION
ORAL SUCTIONING - 4 TH HRLY POSTURAL CHANGE - 2 ND HRLY
Advice at Discharge
TAB. LEVEPIL 500 MG RT / BD X TO CONTINUE TAB. STROCIT PLUS RT/ BD X 15DAYS
TAB. CINOD 10 MG RT/BD X TO CONTINUE
TAB. TELMA-H 40/12.5 MG RT/BD X TO CONTINUE TAB. MET XL 25 MG RT / OD X TO CONTINUE
TAB. THJIAMINE 100MG RT BD X10DAYS SYP.LACTULOSE 15 ML RT/TID
NEB WITH IPRAVENT AND BUDECORT -M 12 TH HRLY PHYSIOTHERAPY OF B/L UPPER AND LOWER LIMBS CHEST PHYSIOTHERAPY
Follow Up
REVIEW TO GM OPD AFTER 1 WEEK / SOS
When to Obtain Urgent Care
IN CASE OF ANY EMERGENCY IMMEDIATELY CONTACT YOUR CONSULTANT DOCTOR OR ATTEND EMERGENCY DEPARTMENT.
Preventive Care
AVOID SELF MEDICATION WITHOUT DOCTORS ADVICE,DONOT MISS MEDICATIONS. In case
of Emergency or to speak to your treating FACULTY or For Appointments, Please Contact: For Treatment Enquiries Patient/Attendent Declaration : - The medicines prescribed and the advice regarding preventive aspects of care ,when and how to obtain urgent care have been explained to me in my own language
SIGNATURE OF PATIENT /ATTENDER
SIGNATURE OF PG/INTERNEE
SIGNATURE OF ADMINISTRATOR
SIGNATURE OF FACULTY
Discharge Date Date: 01/11/24 Ward: AMC Unit:IV