Introduction:
The patient centred learnings in a global academic medical institution has for centuries been reflected in it's rate of pathological autopsies conducted that over the years have unearthed nuggets of useful information from individual patients that in many instances may have been the first signposting of a new disease hitherto unknown to mankind.
To quote:
"The autopsy was not only performed to provide clinicians with the cause of death but to establish the very nature of the pathology which may have been suspected, or to document pathology which was totally unknown during life. From these individual autopsies, the process of systemic analysis of pathologic features with the application of special stains and the addition of increasingly sophisticated techniques culminated in papers in journals. That exercise continues today. One contemporary example of this process which began with the autopsy is the initial cases of a bewildering, catastrophic disease occurring in young men in San Francisco in the early 1980s which we know as human immunodeficiency virus (HIV)-acquired immunodeficiency syndrome"
Coming to the workflow of a particular global Indian institute conducting regular autopsies presented twice weekly in academic sessions, the flipped classroom approach is used for Tuesday posting of the CPC clinical protocol since many decades before some medical educationist even thought of the term for this! https://en.m.wikipedia.
The clinical protocol for initiating the CPC shared on Tuesday.
Although again we suspect most people may not have had the time to go through it before they started viewing the CPC either onsite in the auditorium or through the weblink which also was shared along with the clinical protocol on Tuesday.
Clinical protocol (a lot of it appears to have been retrieved from the patient's EMR and then summarized below):
Staff CPC 25-09-2024
Patient: A, 48/Female
Clinician I/C:
Prof.
CR No:
Clinical Discussant: Dr.
DOA: 15-11-2023,
Radiology discussant:
DOD: 25-11-2023
Pathologist:
Dr.
Presenting complaints: Loose stools, 4-5 episodes per day for two days, accompanied by undocumented low-grade fever. Admitted to a private hospital for altered mental status and managed for ?generalized seizures.
Detected to have high blood sugars (>400 mg/dL) and hyponatremia (124 mmol/L). Dry cough 15-20 days.
Past history: Hypothyroidism, Chronic kidney disease on maintenance hemodialysis since 2020.
Renal transplantation (9-Oct-2023): Live-related renal allograft recipient (donor-husband); Induction – ATG;
Discharged after 9 days (Creatinine 2.06 mg/dL) on tacrolimus, MMF and prednisolone. Tac level – 8.78 ng/mL
(Ref - 10 to 15 ng/mL).
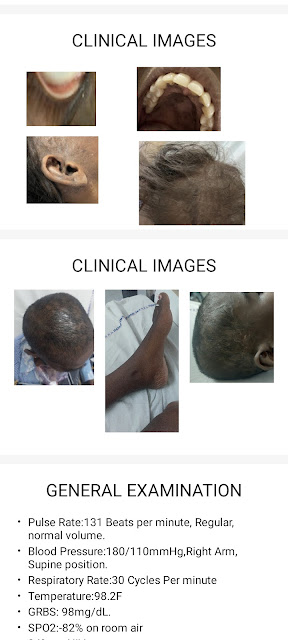
Examination: E2V1M4, BP 150/90, RR 22/minute, HR 110/minute, SpO2 – 98%. B/L pupils, small reacting to
light, no neck rigidity, bilateral plantar flexor. Marginal skin necrosis and pus discharge
Investigations
15/11/23 17/11/23 19/11/23 21/11/23 22/11/23 23/11/23 25/11/23
Complete blood count
Hb, g/dL
7
7.7
7.3
8.1
6
6.2
8
TLC, (*109
/L)
22720
21550
17800
26550
12350
11020
8830
DLC (N/L%)
92/6
90/3
88/8
90/8
88/8
Platelets, (*109
/L)
213
140
24
25
20
16
6
PBF - Mild anisocytosis, Microcytic, hypochromic, tear drop cells, nRBCs, reduced platelets.
Schistocytes insignificant and <1% - two separate reports
Biochemistry
Na/K, mmol/L
144/3.4
145/3.3
157/3.7
148/5.5
147/3.9
146/3.1
144/2.3
BU/Creat, mg/dL
46/1.4
71/1.3
89/1.3
104/1.3
113/1.5
99/1.2
108/1
Bilirubin, mg/dL
0.7
0.6
0.7
0.6
0.7
0.7
1.1
Prot/Alb, mg/dL
7.1/3.4
5.9/2.7
4.8/2.4
4.5/2.4
4.6/2.4
5.4/2.6
5.2/2.5
AST/ALT, U/L
21/29
23/41
29/27
33/38
18/27
25/29
51/49
Alk Phos, U/L
265
199
366
280
314
382
Ca/PO4, mg/dL
9.7/2.6
9.2/3.0
8.7/3.9
9.2/3.5
8.6/4.7
8.9/5.7
Magnesium, mg/dL
1.8
1.4
1.7
1.5
Arterial blood gases
pH
7.42
7.47
7.45
7.39
7.46
PaO2
83
60
84
37
34
PaCO2
10
21
24
30
29
HCO3
6.7
15
17
22
24
FiO2 (on MV)
0.24
0.21
0.21
0.21
0.21
Coagulation profile: PT-10.7 sec, aPTT 31 sec, PTI – 100%, D-dimer – 919 ng/mL (19/11/23 and 21/11/23)
Urine routine: (15/11/23) Sugar - +++ (1000 mg/dL), ketones - + (10mg/dL), blood+++
Urine microscopy: RBCs – 247/hpf (range: 0-2), WBC – 1.4 /hpf (0-4), bacteria-31/hpf (0-80)
ECG- HR 110, ST segment depression and T inversion II, III, aVF, v4-v6
CK MB – 38 U/L (19-Nov-23), Trop T – 53, Pro BNP – 8435 pg/mL
T3-0.379 (0.8-2 pg/mL). T4-5.98 (4.8-12.7 µg/L), TSH – 2.70 (0.27-4.2 µIU/mL)
HbA1C- 7.2%, cortisol-1400 mmol/L
G6PD – normal; plasma Hb – not raised, urine Hb- not detected; Direct Coombs test – negative
Serum galactomannan – 0.12; beta-D-glucan- 37
EEG (21/11/23) – suggestive of encephalopathy; EEG (23/11/23) – Electrical silence
16/11/23
17/11/23
18/11/23
Blood cultures Sterile x 3
ET aspirate
Enterococcus faecium
Aseptate hyphae, Rhizopus arrhizus
Urine cultures
Sterile
Cocci 195/hpf; sterile
Pus g/s, c/s
Enterococcus faecium
CSF
TC/DC – 821/mm3 (N91%, L7%), Protein – 416 mg/dL, Sugar – 86 mg/dL
Culture sterile, fungal smear, India Ink and cryptococcal antigen - negative
Imaging:
USG abdomen (Outside) - gallstone 24 mm, shrunken native kidneys, graft kidney in RIF with 16 mm perinephric
collection anteriorly
USG abdomen – Renal parenchymal disease of transplant kidney, 13*5 mm perinephric collection, prominent
CBD with central IHBRD ?benign stricture
Echo (TTE): Conc LVH, Mobile mass attached to ventral side of PML 8*5 mm; mild MR, no RWMA
Echo (19-Nov-23): RWMA LCX territory, EF-35-40%, mass attached to PML 8*2 mm (?healed lesion or
calcification)
CXR – Right upper zone thick-walled cavity (14/11/23 and 15/11/23)
CT thorax: R upper lobe consolidation with large cavitation and internal septae, patch of consolidation in left LL
NCCT KUB: Transplant kidney in situ with small perinephric collection, air foci within operative site s/o wound
dehiscence, dilated GB, and CBD
CEMRI brain (16/11/23) – diffuse leptomeningeal enhancement s/o meningitis. Large hemorrhagic peripherally
enhancing lesions in bilateral basal ganglia and frontal lobes with perilesional edema and mass effect. Small
abscess in the right occipital lobe
NCCT head (19/11/23) – Diffuse cerebral edema, left PCA territory infarct, tonsilar and transtentorial herniation
Course & Management
A 48-year-old female underwent renal transplantation at a private hospital for CKD-ESRD (diagnosed in
2020, basic disease - unknown). Thirty-five days following transplantation, she developed loose stools, low-grade
fever and was admitted to a private hospital with altered mentation (?preceded by a seizure episode).
Hyperglycemia and hyponatremia were observed. She was admitted to PGI emergency the next day, required
endotracheal intubation for altered sensorium and was later shifted to RICU. Chest radiograph and CT thorax
suggested possible pulmonary mucormycosis, and neuroimaging showed bilateral intracranial lesions
(?hemorrhagic infarcts). Physical examination suggested surgical site infection. She was managed with
intravenous liposomal amphotericin-B, vancomycin and wound debridement. Serum creatinine and urine output
remained stable till demise while thrombocytopenia, leukocytosis and anemia continued to worsen (required
PRBC transfusions). There was no clear evidence of hemolysis or TMA. She was managed for infective
endocarditis based on echocardiography at admission, showing 8*5 mm vegetation in PML. Blood and urine
cultures were sterile, and CSF showed leukocytosis (neutrophilic). On day 4 of the RICU stay, she developed
shock, and a repeat echocardiography showed RWMA and reduced LVEF (30-35%); antiplatelets could not be
administered due to thrombocytopenia. Shock persisted despite vasopressor support. Fever recurred, GCS
worsened, and neuroimaging suggested further deterioration. EEG showed electrical silence (23/11/23), and the
patient suffered a cardiac arrest resulting in her demise (25/11/23).
Unit’s final diagnosis
Post renal transplant status (LERRAR – Oct 2023)
Diabetes mellitus (?New-onset diabetes after transplantation) with diabetic ketoacidosis
Disseminated (Pulmonary and cerebral) mucormycosis
Surgical site infection – Enterococcus spp.
Infective endocarditis ?fungal
Inferior wall myocardial infarction
Severe sepsis, septic and cardiogenic shock
Cause of death
Raised intracranial tension
The web link invite to view it from global individual nodes, along with the clinical summary that is circulated on social media is similar to what is pasted below:
Greetings.
The next Wednesday CPC of the session will be held on September 25, 2024 at 08.00 hours (IST) in Lecture Theatre 1, Nehru Hospital, PGIMER, Chandigarh.
The session will also be available on the Webex platform. Kindly follow the link below to join.
In case you join in thru WebEx, kindly ensure that your microphone and camera are switched off and PLEASE DO NOT SHARE YOUR SCREEN.
Then on Wednesday we have the actual CPC that looks something like this (this is taken from their past publicly available records archived in YouTube as the video of the presentation in the protocol above isn't yet ready) if you are viewing it through the weblink:
And then we have this user driven learning community UDLC discussion (UDLCO Transcripts) around the CPC in global social media alumni groups such as the one pasted below:
[25/09, 09:12] NJ:
Interesting CPC.
Some observations
1) too many abbreviations
2) how was the diagnosis of DKA made? I only see one urine ketone measurement of 1+ - which is not pathognomonic of KA.
3) no mention of how the DKA was treated.
4) did the pathologist present the histology of pancreas? Is immunostaining for insulin informative in NODAT?
Pathology autopsy results are shared into the global alumni group discussion at this point by S:
Illustrative sample of autopsy organs image shared with a creative commons license from:https://commons.m.
[25/09, 10:35] NJ: Thanks S!
If the pancreatic pathology supports bronze diabetes (hemochromatosis-induced DM), it’s all the more difficult to explain DKA. Typically, despite having selective loss of beta cells, the glucagon excess doesn’t translate to increased ketogenesis because the insulin deficiency is usually not absolute.
[26/09, 08:16] CBBLE moderator: Yes it's quite rare👇
[26/09, 08:30] CBBLE moderator commenting on the autopsy: Even in the destroyed native kidneys there were islands of viable glomerular mesangial proliferation noted that appears to have been subjected to DIF and findings were just mentioned as similar.
So overall the main culprit in this story
(as also expounded by the original discoverers of PGMID here: https://www.ncbi.nlm.nih.gov/
appears the IgG3, which composes only 8% of IgG in the circulation, has several properties that allow it to be intrinsically “nephritogenic.” It is the most positively charged subclass (pI 8.2 to 9.0), favoring affinity for intrinsic anionic sites in the GCW. It has the highest molecular weight (170,000 Da), making it more size-restricted by the glomerular filtration barrier.
Thus, in the course of filtration, the intra capillary concentration of circulating IgG3 would be predicted to rise, promoting the potential for intraglomerular aggregation. (Unquote).
However this doesn't still explain the secondary hemosiderosis?
[26/09, 09:53] NJ: I thought they said that iron overload would have happened during dialysis prior to the transplant.
[26/09, 14:52] CBBLE moderator: Yes so perhaps it was just incidental pathological changes due to that without much functional significance as prior documented here:
and the diabetes and DKA was due to "developing new-onset diabetes mellitus after transplantation (NODAT). The risk of NODAT has been reported to be as high as 32% after a solid organ transplant.Diabetic ketoacidosis develops in approximately 8% of patients with NODAT."
Unquote
[26/09, 19:07] NJ: Yes, agree if it was NODAT.
I’m wondering at the diagnosis of DKA. What was the evidence? What was the treatment? There’s nothing in the case summary to support it.
Some references and memories of CPC stalwarts from the particular institute featured in this write up in the link below:
UDLCO keyword glossary: