Our first clinical encounter with her was in 5/11/2022 and borrowing from the student's online learning portfolio (who documented the initial encounter at the time here: https://rishithareddy30.
"History of presenting illness:
patient was apparently normal till six years back in 2017 she had generalised body aches and joint pains which involves multiple large joints of which elbow And knee joints troubled her associated with generalised body aches after multiple hospital visits
she even noticed hair loss without scarring and oral ulcers then she was diagnosed with autoimmune disorder and initiated on hydroxychloroquine azathioprine wysolone
she reported that her joint pains and hair loss was not improving with the above medication she had multiple hospital visits and admissions for joint pains and body aches which bothers her from doing her activities .
Two months back she had pedal edema two months back she had pedal edema sudden onset shortness of breath initially on exertion then she was diagnosed with hypertensive emergency admitted and discharged with antihypertensive . patients stopped AZA as advised by doctor except hyper antihypertensive since yesterday she had shortness of breath initially on exertion which rapidly progressed to sob at rest."
Two more students from the same batch:
2022 EMR discharge summary:
Age/Gender : 31 Years/Female
Address :
Discharge Type: Relieved
Admission Date: 05/11/2022 11:02 PM
Diagnosis
ACUTE CARDIOGENIC PULMONARY EDEMA SECONDARY TO CHRONIC RENAL FAILURE SECONDARY TO ?SLE /LUPUS NEPHRITIS
SEIZURES SECONDARY TO ?CNS VASCULITIS /?UREMIC
Discharge Type: Relieved
Admission Date: 05/11/2022 11:02 PM
Diagnosis
ACUTE CARDIOGENIC PULMONARY EDEMA SECONDARY TO CHRONIC RENAL FAILURE SECONDARY TO ?SLE /LUPUS NEPHRITIS
SEIZURES SECONDARY TO ?CNS VASCULITIS /?UREMIC
Case History and Clinical Findings
PT CAME WITH C/O SOB SINCE MORNING ON 5/11/22 C/O VOMITINGS 2 EPISODES
K/C/O SLE SINCE 2017 ON REGULAR MEDICATION K/C/O HTN SINCE 1 MONTH ON REGULAR MEDICATION N/K/C/O DM,ASTHMA,EPILEPSY,TB
PATIENT WAS APPARENTLY ASYMPTOMATIC 6 YEARS BACK
IN 2017 SHE HAD GENERALISED BODYACHES AND JOINT PAINS WHICH INVOLVED MULTIPLE LARGE JOINTS OF WHICH ELBOW AND KNEE JOINT ACHES TROUBLED HER ASSOSCIATED WITH GENERALISED BODY ACHES
AFTER MULTIPLE HOSPITAL VISITS SHE EVEN NOTICED HAIR LOSS WITHOUT SCARRING AND ORAL ULCERS
THEN SHE WAS DIAGNOSED WITHAUTOIMMUNE DISORDER SLE AND INITIATED ON HCQ
,AZATHIOPRINE AND WYSOLONE .
SHE REPORTED THAT HER JOINT PAINS AND HAIRLOSS WAS NOT IMPROVING WITH ABOVE MEDICATION
2 MONTHS BACK SHE HAD PEDAL EDEMA AND SUDDEN ONSET OF SHORTNESS OF BREATH INITIALLY ON EXERTION THEN WORSENED TO EVEN AT REST
SHE WAS DIAGNOSED WITH HYPERTENSIVE EMERGENCY ADMITED AND DISCHARGED WITH ANTIHYPERTENSIVES
SINCE 10 DAYS PATIENT STOPPED TAKING ALL HER MEDICATIONS EXCEPT ANTIHYPERTENSIVES
SINCE YESTERDAY[4/11/22] SHE HAD SHORTNESS INITIALLY ON EXERTION WHICH RAPIDLY PROGRESSED TO SOB AT REST
NO SMALL JOINTS PAINS NO COLOUR CHANGE /PARAESTHESIAS OF FINGERS ON EXPOSURE TO COLD
PT HAD 1 EPISODE OF INVOLUNTARY MOVEMENTS INITIALLY STARTED LEFT HAND FOLLOWED BY TOTAL BODY WITH IMPAIRED CONSCIOUSNESS
NO TONGUE BITE ,NO INVOLUNTARY MICTURITION /DEFECATION
ON EXAMINATION
PT IS CONSCIOUS COHERENT COOPERATIVE ON PRESENTATION
VITALS
BP 220/140 MMHG PR 134 BPM
RR 36CPM SPO2 52 ON RA
GRBS 236 MG /DL
GENERAL PHYSICAL EXAMINATION PALLOR +
FLAT NAILS
NON SCARRING ALOPECIA
HYPERPIGMENTED DISCOID RASHES ON FACE PERIAURAL BLACK DISCOLORATION OF ORAL MUCOSA AND PALATE MILD PEDAL EDEMA
CVS
NO RAISED JVP S1S2+
NO MURMURS RS
BAE +
DIFFUSE INSPIRATORY AND EXPIRATORY CREPTS +
P/A SOFT NON TENDER MILD DISTENDED UMBILICUS INVERTED NO ORGANOMEGALY CNS
HMF INTACT E4V5M6 PUPILS NSRL NO FND
LAST SEIZURES 4/11/22 COURSE IN HOSPITAL
4 SESSIONS OF DIALYSIS DONE OPHTHA REFERAL ON 5/11/22
IMPRESSION- NO CHANGES ON FUNDUS EXAMINATION DVL REFERAL ON 7/11/22
DIAGNOSIS-SYSTEMIC LUPUS ERYTHEMATOSUS +CICATRICIAL ALOPECIA TREATMENT-TACROS OINT 0,03% L/A /OD FOR 2 WEEKS
PHOTO BAN AQUA GEL L/A [9AM-12PM-3PM] RENAL BIOPSY DONE ON 12/11/22
Investigation
CBP HB TC N L E M B PLT SMEAR RFT UR CR UA CA+2 P NA+ K+ CL- HIV HBSAG HCV MDCT SCAN BRAIN PLAIN
IMPRESSION-
F/S/O HYPERTENSIVE ENCEPHALOPATHY /POSTERIOR REVERSIBLE ENCEPHALOPATHY[PRES]
Treatment Given(Enter only Generic Name)
INJ LEVIPIL 500 MG /IV/TID
INJ NTG 50 MG IN 50 ML NS @5ML/HR INC /DEC TO MAINTAIN SBP <160 MMHG[STOPPED ON 07/11/22]
INJ LASIX 40 MG/IV/BD INJ HAI S/C ACC TO GRBS
TAB .NICARDIA RETARD 20 MG /PO/QID TAB OROFER XT PO/OD
TAB HCQ 200 MG PO/BD
TAB METXL 50 MG PO/BD TAB TELMA 40 MG PO/OD
TAB WYSOLONE 20 MG /PO/OD TAB HYDRALAZINE 12.5 MG PO/TID TAB PCM 650 MG/PO/QID
TAB DEPINE 5MG /PO/QID FLUID AND SALT RESTRICTION
Advice at Discharge
TAB LEVIPIL 500 MG PO/'BD TAB LASIX 40 MG PO/BD
TAB .NICARDIA RETARD 20 MG /PO/QID TAB OROFER XT PO/OD
TAB METXL 50 MG PO/BD TAB TELMA 40 MG PO/OD
TAB WYSOLONE 20 MG /PO/OD TAB PCM 650 MG/PO/QID
TAB ULTRACET 1/2 TAB PO/QID[1/2-1/2-1/2-1/2] FLUID AND SALT RESTRICTION
When to Obtain Urgent Care
IN CASE OF ANY EMERGENCY IMMEDIATELY CONTACT YOUR CONSULTANT DOCTOR OR ATTEND EMERGENCY DEPARTMENT.
Preventive Care
AVOID SELF MEDICATION WITHOUT DOCTORS ADVICE,DONOT MISS MEDICATIONS. In case
of Emergency or to speak to your treating FACULTY or For Appointments, Please Contact: For Treatment Enquiries Patient/Attendent Declaration : - The medicines prescribed and the advice regarding preventive aspects of care ,when and how to obtain urgent care have been explained to me in my own language
SIGNATURE OF PATIENT /ATTENDER SIGNATURE OF PG/INTERNEE SIGNATURE OF ADMINISTRATOR SIGNATURE OF FACULTY
Discharge Date Date:14/11/22 Ward:NEPHRO WARD
2023 discharge summary :
Date of admission: 06/02/2023 02:37 PM
Diagnosis
Diagnosis
ACUTE KIDNEY INJURY ON CHRONIC KIDNEY DISEASE [LUPUS NEPHRITIS STAGE 1V/V] SECONDARY TO ACUTE GASTROENTERITIS [ RESOLVED ]
WITH HYPERKALEMIA [ RESOLVED ]
WITH ? ANEMIA OF CHRONIC INFLAMMATION WITH ? ANEMIA INDUCED HEART FAILURE WITH ? ACUTE PULMONARY EDEMA [RESOLVED]
Case History and Clinical Findings
CHIEF COMPLAINTS :
C/O VOMITING AND LOOSE STOOLS SINCE 3 DAYS HOPI :
PT WAS APPRENTLY ASYMPTOMATIC 3 DAYS AGO THEN SHE DEVELOPED LOOSE STOOLS 3-4 EPISODES / DAY , WATERY CONSISTENCY , NOT ASSOCIATED WITH FEVER , PAIN ABDOMEN
C/O VOMITINGS SINCE 3 DAYS 2-3 EPISODES PER DAY CONTAINED FOOD PARTICLES INITIALLY THEN HAD YELLOWISH COLOR VOMITINGS , NON FOUL SMELLING , NON BLOOD STAINED
K/C/O SLE WITH LUPUS NEPHRITIS SINCE 2 MONTHS AND IS ON TAB HCQ 200MG IS ON RABEPRAZOLE + DOMPRIDONE 7AM
T.OROFER XT PO/OD 8AM T.SHELCAL 500MG PO/OD 8AM
T.SODIUMBICARBONATE 500MG PO/BD 2PM AND 8PM T.NICARDIA 20MG PO/TID 8AM-2PM-8PM T.NEPHROSAVE PO/OD 2PM
PROBIOTICS
N/K/C/O DM , ASTHMA , EPILEPSY , CAD , CVA , THYROID DISORDERS K/C/O HTN SINCE 3 MONTHS
NO PAST SURGICAL HISTORY MENSTRUAL CYCLE :
IRREGULAR SINCE 2 MONTHS LMP - 25TH DECEMBER 2022
O/E:
PT. IS C/C/C
NO PALLOR,ICTERUS,CYANOSIS,
BP-180/110MMHG PR-131BPM
RR-24CPM RBS-118MG/DL
CVS-S1S2+,NO MURMURS RA-BAE+,NVBS
P/A-SOFT, TENDERNESS AROUND UMBLICUS , BOWEL SOUNDS HEARD CNS-NO FND
OPTHALMOLOGY OPINION WAS TAKEN I/V/O HYPERTENSIVE RETINOPATHY CHANGES AND NO HYPERTENSIVE CHANGES WERE NOTED
GYNECOLOGY OPINION WAS TAKEN I/V/O AMENORRHOEA SINCE 3 MONTHS AND ENT OPINION WAS TAKEN I/V/O DYSPHAGIA AND WAS DIAGNOSED ODYNOPHAGIA SECONDARY TO GASTRITIS
BLOOD TRANSFUSION OF 1 PRBC WAS DONE ON 13/2/23 IV/O LOW HEMOGLOBIN NEPHROLOGY OPINION WAS TAKEN I/V/O OF RASIED SERUM CREATINE AND UREA LEVELS AND WAS ADVICED HEMODIALYSIS
HEMODIALYSIS WAS DONE ON 16/2/23 AND 17/2/23
Investigation
USG ABDOMEN AND PELVIS ON 06/2/23
B/L RAISED ECHOGENECITY IN BOTH KIDNEYS MILD ASCITIS
USG ABDOMEN AND PELVIS ON 9/2/23
GB WALL EDEMA NOTED MEASURING 8MM
MILD RIGHT PLEURAL EFFUSION , MINIMAL LEFT PLEURAL EFFUSION IVC DIAMETER MAX 18MM MIN 16MM
DILATED HEPATIC VEINS NOTED MINIMAL PERICARDIAL EFFUSION FEATURES SUGGESTIVE OF SEROSITIS HEMOGRAM
HB - 4.4-6.7-6.1-5.9-6.0-6.3-8.5-8.
TLC - 5500-3400-5960-6980-6190-8700-
Treatment Given(Enter only Generic Name)
IV FLUIDS NS AT 100ML/HR NEB WITH DUOLIN 6TH HRLY INJ PAN 40MG IV/OD
INJ ZOFER 4MG IV/SOS INJ LASIX 40MG IV/BD
INJ METROGYL 500MG IV /TID
INJ METHYLPREDNISOLONE 1GM IV/OD INJ NTG 2CC IV GIVEN
TAB NICARDIA 10MG PO/SOS TAB CLINIDIPINE 10MG PO/BD TAB WYSOLONE 40MG PO/OD TAB SPOROLAC DS PO/BD TAB HCQ 200MG PO/OD
TAB AZATHIOPRINE 50MG PO/OD
SYP SUCRALFATE 10ML TID BEFORE FOOD TAB MET XL 25MG PO/OD
Advice at Discharge
TAB NICARDIA 30MG AT 8AM , 20MG AT 2PM , 30MG AT 8PM TAB HCQ 200MG PO/OD
TAB MET-XL 25MG PO/OD
TAB AZATHIPRINE 50MG PO/OD
TAB WYSOLONE 30MG/PO OD 20MG AT 8AM 10MG AT 6PM TAB PAN 40MG PO/OD
TAB ZOFER 4MG PO/SOS TAB LASIX 40MG PO/TID
SYP SUCRALFATE 10ML PO/TID BEFORE MEALS
Follow Up
REVIEW SOS OR AFTER 1 WEEK TO GENERAL MEDICINE OPD
When to Obtain Urgent Care
IN CASE OF ANY EMERGENCY IMMEDIATELY CONTACT YOUR CONSULTANT DOCTOR OR ATTEND EMERGENCY DEPARTMENT.
Preventive Care
AVOID SELF MEDICATION WITHOUT DOCTORS ADVICE,DONOT MISS MEDICATIONS. In case
of Emergency or to speak to your treating FACULTY or For Appointments, Please Contact: For Treatment Enquiries Patient/Attendent Declaration : - The medicines prescribed and the advice regarding preventive aspects of care ,when and how to obtain urgent care have been explained to me in my own language
SIGNATURE OF PATIENT /ATTENDER SIGNATURE OF PG/INTERNEE SIGNATURE OF ADMINISTRATOR SIGNATURE OF FACULTY
Discharge Date Date:14/2/23 Ward:AMC
Unit: 1
PT. IS C/C/C
NO PALLOR,ICTERUS,CYANOSIS,
BP-180/110MMHG PR-131BPM
RR-24CPM RBS-118MG/DL
CVS-S1S2+,NO MURMURS RA-BAE+,NVBS
P/A-SOFT, TENDERNESS AROUND UMBLICUS , BOWEL SOUNDS HEARD CNS-NO FND
OPTHALMOLOGY OPINION WAS TAKEN I/V/O HYPERTENSIVE RETINOPATHY CHANGES AND NO HYPERTENSIVE CHANGES WERE NOTED
GYNECOLOGY OPINION WAS TAKEN I/V/O AMENORRHOEA SINCE 3 MONTHS AND ENT OPINION WAS TAKEN I/V/O DYSPHAGIA AND WAS DIAGNOSED ODYNOPHAGIA SECONDARY TO GASTRITIS
BLOOD TRANSFUSION OF 1 PRBC WAS DONE ON 13/2/23 IV/O LOW HEMOGLOBIN NEPHROLOGY OPINION WAS TAKEN I/V/O OF RASIED SERUM CREATINE AND UREA LEVELS AND WAS ADVICED HEMODIALYSIS
HEMODIALYSIS WAS DONE ON 16/2/23 AND 17/2/23
Investigation
USG ABDOMEN AND PELVIS ON 06/2/23
B/L RAISED ECHOGENECITY IN BOTH KIDNEYS MILD ASCITIS
USG ABDOMEN AND PELVIS ON 9/2/23
GB WALL EDEMA NOTED MEASURING 8MM
MILD RIGHT PLEURAL EFFUSION , MINIMAL LEFT PLEURAL EFFUSION IVC DIAMETER MAX 18MM MIN 16MM
DILATED HEPATIC VEINS NOTED MINIMAL PERICARDIAL EFFUSION FEATURES SUGGESTIVE OF SEROSITIS HEMOGRAM
HB - 4.4-6.7-6.1-5.9-6.0-6.3-8.5-8.
TLC - 5500-3400-5960-6980-6190-8700-
Treatment Given(Enter only Generic Name)
IV FLUIDS NS AT 100ML/HR NEB WITH DUOLIN 6TH HRLY INJ PAN 40MG IV/OD
INJ ZOFER 4MG IV/SOS INJ LASIX 40MG IV/BD
INJ METROGYL 500MG IV /TID
INJ METHYLPREDNISOLONE 1GM IV/OD INJ NTG 2CC IV GIVEN
TAB NICARDIA 10MG PO/SOS TAB CLINIDIPINE 10MG PO/BD TAB WYSOLONE 40MG PO/OD TAB SPOROLAC DS PO/BD TAB HCQ 200MG PO/OD
TAB AZATHIOPRINE 50MG PO/OD
SYP SUCRALFATE 10ML TID BEFORE FOOD TAB MET XL 25MG PO/OD
Advice at Discharge
TAB NICARDIA 30MG AT 8AM , 20MG AT 2PM , 30MG AT 8PM TAB HCQ 200MG PO/OD
TAB MET-XL 25MG PO/OD
TAB AZATHIPRINE 50MG PO/OD
TAB WYSOLONE 30MG/PO OD 20MG AT 8AM 10MG AT 6PM TAB PAN 40MG PO/OD
TAB ZOFER 4MG PO/SOS TAB LASIX 40MG PO/TID
SYP SUCRALFATE 10ML PO/TID BEFORE MEALS
Follow Up
REVIEW SOS OR AFTER 1 WEEK TO GENERAL MEDICINE OPD
When to Obtain Urgent Care
IN CASE OF ANY EMERGENCY IMMEDIATELY CONTACT YOUR CONSULTANT DOCTOR OR ATTEND EMERGENCY DEPARTMENT.
Preventive Care
AVOID SELF MEDICATION WITHOUT DOCTORS ADVICE,DONOT MISS MEDICATIONS. In case
of Emergency or to speak to your treating FACULTY or For Appointments, Please Contact: For Treatment Enquiries Patient/Attendent Declaration : - The medicines prescribed and the advice regarding preventive aspects of care ,when and how to obtain urgent care have been explained to me in my own language
SIGNATURE OF PATIENT /ATTENDER SIGNATURE OF PG/INTERNEE SIGNATURE OF ADMINISTRATOR SIGNATURE OF FACULTY
Discharge Date Date:14/2/23 Ward:AMC
Unit: 1
Finally this month presented in the meeting circulated here:
INTEGRATED MEET CASE PRESENTATION
DR.JYOTHULA HARIPRIYA
FINAL YEAR POSTGRADUATE
DEPARTMENT OF GENERAL MEDICINE
DR.JYOTHULA HARIPRIYA
FINAL YEAR POSTGRADUATE
DEPARTMENT OF GENERAL MEDICINE
CHIEF COMPLAINTS
A 30 years old woman , resident of , ... by occupation came with chief complaints of:
Swelling of both lower limbs since 3 days.
Decreased urine output since 1 day.
Shortness of breath since 1 day.
HISTORY OF PRESENT ILLNESS
Patient was apparently asymptomatic 3 days back and then she had swelling of both lower limbs,which is insidious in onset, gradually progressive ,pitting type, initially started around ankle and extended till knee associated with facial puffiness and dry cough more on lying down position.
Decreased urine output since 1day.
Shortness of breath since 1 day ,insidious in onset ,gradually progressive, from MMRC grade 2 to grade 4[worsened since 30 minutes].
Sudden onset of shortness of breath since 30minutes.
HISTORY OF PRESENT ILLNESS
Orthopnoea and PND present.
No h/o fever, Cold, Cough.
No h/o pain abdomen, Vomiting, Loose stools.
No h/o chest pain,palpitations.
No history of burning micturition
PAST HISTORY
TIMELINE OF EVENTS
PAST HISTORY
K/C/O Hypertension since 7 months and was on medication, Tab. Nicardia 30mg PO TID
K/C/O SLE since 6 years used Rx for 5 years and stopped.
Renal biopsy done on 12/11/2022 - Diagnosed with Lupus Nephritis [restarted on Rx].
Not a k/c/o Diabetes mellitus, Thyroid, Coronary artery disease, Cerebrovascular accident.
PERSONAL HISTORY
Mixed diet
Appetite decreased.
Bowel habits regular
Decresed urine output since 1 day.
Sleep adequate.
No allergies
Addictions: Nil.
GENERAL EXAMINATION
Patient is consious and coherent at the time of presentation.
Poorly built and nourished.
Pallor present
Edema +[Both lower limbs]
Buccal pad of fat lost.
JVP: Raised
GENERAL EXAMINATION
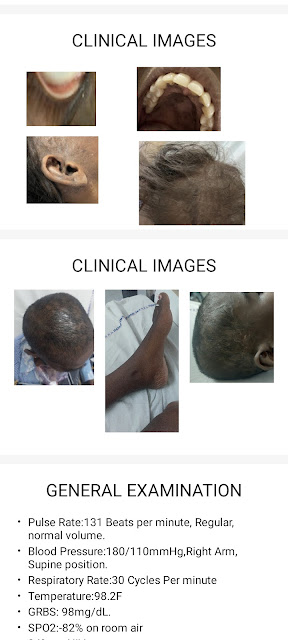
Non scarring alopecia present
Hyper pigmented discoid rashes over the face
Black discoloration of oral mucosa and palate.
No icterus, Cyanosis, Clubbing, Koilonychia, Lymphadenopathy.
CLINICAL IMAGES
GENERAL EXAMINATION
Pulse Rate:131 Beats per minute, Regular, normal volume.
Blood Pressure:180/110mmHg,Right Arm, Supine position.
Respiratory Rate:30 Cycles Per minute
Temperature:98.2F
GRBS: 98mg/dL.
SPO2:-82% on room air
94% on NIV
SYSTEMIC EXAMINATION
RESPIRATORY SYSTEM :
Inspection:
Chest is elliptical shaped, Bilaterally symmetrical.
Trachea is central.
Movements are equal on both sides.
No scars, sinuses or visible pulsation.
SYSTEMIC EXAMINATION
RESPIRATORY SYSTEM:
Palpation:
All inspectory findings are confirmed :Trachea is central.
Apex beat felt in left 6th Intercostal space lateral to mid clavicular line.
Vocal fremitus felt equally in all areas
SYSTEMIC EXAMINATION
RESPIRATORY SYSTEM:
Percussion:
All areas are resonant on percussion
Auscultation:
Bilateral air entry present
Normal vesicular breath sounds heard.
Fine end inspiratory and expiratory crepitations heard all over the chest[more in bilateral basal regions].
SYSTEMIC EXAMINATION
CARDIOVASCULAR SYSTEM:
Elliptical and Bilaterally symmetrical chest
No visible pulsations/engorged veins/scars/sinuses on chest wall.
Apex beat palpable at left 6th Intercostal space lateral to mid clavicular line.
S1 and S2 heard
JVP raised.
No Murmurs,No parasternal heave.
SYSTEMIC EXAMINATION
PER ABDOMEN :
On inspection:
Scaphoid.
Umbilicus inverted.
All quadrants are moving equally with respiration.
No visible pulsations/engorged veins/scars/sinuses.
SYSTEMIC EXAMINATION
Palpation:
Soft and non tender.
No organomegaly.
No palpable masses.
Percussion:
Tympanic note felt.
Auscultation:
Bowel sounds are heard.
No para aortic briut.
SYSTEMIC EXAMINATION
CENTRAL NERVOUS SYSTEM:
Patient is consious and oriented.
Bilateral pupils Normal size and reactive to light .
Sensory system : Intact
Motor System :Normal
Reflexes: Elicited and normal.
Cranial Nerves: Functional
PROVISIONAL DIAGNOSIS
Acute pulmonary edema secondary to Heart failure.
K/c/o SLE with lupus nephritis and on maintenance hemodialysis.
K/c/o Hypertension.
INVESTIGATIONS
ECG at Admission :
INVESTIGATIONS
CHEST
X RAY
INVESTIGATIONS
INVESTIGATIONS
ABG
PH :7.27
PCO2 :19
PO2 :53.5
SO2 :82
HCO3 :7
INVESTIGATIONS
IINVESTIGATIONS
INVESTIGATIONS
KIDNEY BIOPSY
Showed features of chronic renal disease, Tubular injury with significant global glomerulosclerosis, interstitial inflammation and mild arteriosclerosis.
Features suggestive of chronic glomerulonephritis –Lupus nephritis.
2D ECHO
Dilated RA,RV,LA,LV.
Concentric LVH,no RWMA.
IVC Dilated and non collapsing.
Ejection fraction 45%.
Moderate MR,TR.
Mild to moderate AR.
Moderate LV systolic function
Diastolic dysfuntion +.
USG ABDOMEN
FINAL DIAGNOSIS
Acute cardiogenic pulmonary edema
Chronic kidney disease secondary to lupus nephritis [stage iv/v]
Anemia of chronic disease
K/c/o SLE and Hypertension since 7 months.
TREATMENT
FLUID AND SALT RESTRICTION
TAB.PREDNISOLONE 5MG PO OD
TAB.NICARDIA 30MG/PO//BD
TAB.ARKAMINE 0.1MG/PO/TID
TAB.METAPROLOL 50MG/PO/OD
TAB.SHELCAL CT /PO/OD
TAB.LASIX 40MG/PO/TID
TAB.NODOSIS 500MG/PO/BD
INJ.ERYTHROPOITIN 4000IU/SC/TWICE WEEKLY.
PATIENT WAS ON MAINTANANCE HEMODIALYSIS WITH REGULAR BLOOD TRANSFUSIONS.
COURSE IN THE HOSPITAL
Patient came with complaints of shortness of breath,swelling of both lower limbs and decreased urine output,and clinically and X ray showed features suggestive of flash pulmonary edema , emergency dialysis was done and patient got improved clinically.
FOLLOW UP
Patient is on follow up and is on maintenance hemodialysis .
Last visit on 5-01-2024.
Died outside the hospital.
THANK YOU